(Browne 2016) VICE News.
Anna Pillipow
The author holds a Bachelor’s Degree in International Studies from the University of Saskatchewan, and Master of Arts in Interdisciplinary Studies with a focus in Global Change from Athabasca University. She works for the Vancouver Island Health Authority (VIHA) in Mental Health and Addiction, while pursuing a Master of Arts in Counselling Psychology from Yorkville University.
This article proposes that it is important that the opioid crisis be understood as an addiction crisis, rather than a crime-related crisis and that viewing it within the framework of health may produce better solutions than trying to effect change through strategies associated with wrongdoing requiring criminal justice as currently exist. It is recommended that Canadian legislation adopt the Portuguese model of public health/ harm reduction to address the opioid crisis in Canada and explores why this may not have happened in the Canadian context. The solutions proposed here that take inspiration from the Portuguese approach include the decriminalization of all drugs, increased access to medical care (detox facilities, treatment beds and transitional housing), as well as integrative work programs in the formal economy. Canada’s current legislation around illicit substances is rooted in racialized immigration ideology and exploitative labor dependencies from the early 20th century. It is time Canada ends its own “war on drugs”.
Keywords: Canada, war on drugs, opioid crisis, harm reduction policies, Portugal.
“Canada has one of the highest per capita consumption of prescription opioids in the world. Dispensing of medications has substantially increased in Canada, although patterns vary considerably between provinces. In 2011, while opioid consumption for medical purposes in morphine equivalence (ME) was 62mg per person globally, Canada’s ME was 812mg per person.” (Canadian Medical Association, 2015, p.1)
Canada is in the midst of an opioid epidemic. Between January 2016 and September 2018 10, 337 peopled died as a result of opioid overdose. From January 2018 through September 2018 Canadians overdosed 3, 286 times (Young 2019). Between 2016 to 2017, there were record numbers that averaged 17 opioid- related hospitalization in-takes per day (Corace 2019, p. 1). However, medical emergencies associated with fentanyl and fentanyl analogues are only part of Canada’s addiction epidemic. Critically, 75% of accidental overdoses involved one or more types of inebriants, including alcohol (Corace 2019, p. 2). This paper argues that it is important that the opioid crisis be understood as an addiction crisis, rather than a crime-related crisis and that viewing it within the framework of health may produce better solutions than trying to affect change through strategies associated with wrongdoing requiring criminal justice as currently exist.
Canadian legislation has channeled billions of dollars per annum into policing and criminal justice to battle drug addiction, instead of public health and rehabilitation, which has been successful in other countries (Felix 2017, Santos 2010 and 2012, Grenfell 2012). For instance, Portugal decriminalized all drugs for individual use in 2001 under a harm reduction model that reframed their opioid crisis as a public health crisis. Funds were rerouted to the Ministry of Health instead of criminal justice. By 2015, overdose deaths had decreased over 80%; new HIV/AIDS diagnoses dropped from 52% to 6%; incarceration for drug offenses decreased by over 40% (Drug Policy Alliance, 6). In other words, the Portuguese model of harm reduction produces positive results. This paper recommends that Canadian legislation adopt the Portuguese model of public health/ harm reduction to address the opioid crisis in Canada and explores why this may not have happened in the Canadian context. The solutions proposed here that take inspiration from the Portuguese approach include the decriminalization of all drugs, increased access to medical care (detox facilities, treatment beds and transitional housing), as well as integrative work programs in the formal economy.
Addiction is a brain disorder heavily influenced by psychosocial elements; addiction, in other words should be viewed as an illness. The DSM-5, which is the diagnostics and statistics manual for mental disorders published by the American Psychiatric Association, recognizes it as such: “… substance use disorder is used to describe the wide range of the disorder, from a mild form to a severe state of chronically relapsing, compulsive drug taking.” (230-231) In other words, substance use disorder can be thought of along a spectrum of severity; a person’s relationship to substance use can progress if untreated, or regress into abstinence. Many people suffering with a severe addiction require multi-faceted care for successful rehabilitation. In the book In the Realm of Hungry Ghosts: Close Encounters with Addiction, author Gabor Maté M.D. defines addiction around four central points: “1. compulsive engagement with the behavior, a preoccupation with it; 2. impaired control over the behavior; 3. persistence or relapse, despite evidence of harm; and, 4. dissatisfaction, irritability or intense craving when the object— be it a drug, activity or other goal— is not immediately available.” (p. 128-129). However, the integrated components of addiction are complex, and Maté makes this clear by writing, “…we need to avoid the trap of believing that addiction can be reduced to the actions of brain chemicals… Addiction has biological, chemical, neurological, psychological, medical, emotional, social, political, economic and spiritual underpinnings…” (p. 129-130). Addiction has a deep interconnection to earlier traumas and stress triggers as a cause for initial use, continued dependency, and relapse based upon the central elements of uncertainty, lack of information, loss of control, emotional isolation and unhealthy relationships. Self-medication becomes a coping mechanism for adverse life experiences, including earlier trauma (Maté 2012). Substance use disorder is a complex pathology and a life-threatening disease, even in the acute stages of withdrawal. For example, acute alcohol and GHB withdrawal needs to be medically supervised, as both substances (and the lack of them under addicts) can cause seizures and/or death. Wrap around medical care is needed to address the root causes of addiction. Throughout this paper wrap around medical care is to be understood as access to detoxification facilities with immediate intake into a treatment center, followed by transitional housing and employment programs.
The opioid crisis in Canada draws resources from two primary fiscal avenues: criminal justice and health care. In 2013, the Office of the Parliamentary Budget Officer completed its first Expenditure Analysis of Criminal Justice in Canada for 2011- 2012. The total per annum expenditure on criminal justice was $20 billion dollars (1). Incarcerating an individual for one year in a provincial correctional facility is approximately $67,000. Monitoring a person on probation or parole cost an average of $18,000 per year (John Howard, 2018). In 2014, $9 billion dollars of criminal justice expenditures were associated with Substance Use (SU). The breakdown is as follows:
By Contrast in 2014, SU health care costs were $11.1 billion; Opioid crisis costs were $313 million (Canadian Substance Use Costs and harms 2018, 2). This is in addition to the damage individuals, families, and communities sustain. For example, it costs $45,000 a year to keep a child in care in Canada (John Howard, 2018).
Part of substance use disorder is defined by a loss of control and use despite the risks. Thus, it is reasonable to conclude that the consequence of incarceration is not an effective deterrent. A punitive approach addresses the symptoms of the problem, but not the underlying cause. Canadian policy could therefore benefit from taking a medical approach to addressing addiction instead of a criminal one. For example, inebriant consumption patterns six months prior to offenders’ (most recent) arrest and incarceration across Canada are as follows: marijuana 85%; alcohol and drugs 80%; cocaine 60%; tranquillizers 35%; opiates 30%; hallucinogens 25%; stimulants 25%; sedatives 20%; heroin 15%; inhalants 5% (Canadian Center on Substance Abuse, 2004). If the addiction is not adequately addressed, then a cyclical relationship begins to form between consumption, compulsion, and acquisition. The Canadian Center on Substance Abuse states that,
The extent to which substance abuse and criminal behaviour are linked increases dramatically with the severity of offenders’ problems. Of those offenders with severe problems, 97% reported that they used on the day of the offence; 87% reported that substance abuse was associated with their crimes over the course of their criminal history. Offenders with more serious substance abuse problems are more likely to be readmitted to custody following release. (2004)
Decreasing criminality, deviant behavior, and addiction requires wrap around medical care that rehabilitates people, allowing individuals to access evidenced-based healthcare approaches to addiction and recovery so individuals can reintegrate and become healthy members of society.
“Harm reduction is a set of practical strategies and ideas aimed at reducing negative consequences associated with drug use. Harm Reduction is also a movement for social justice built on a belief in, and respect for, the rights of people who use drugs. Harm reduction incorporates a spectrum of strategies from safer use, to managed use, to abstinence, to meet drug users “where they’re at,” addressing conditions of use along with the use itself. Because harm reduction demands that interventions and policies designed to serve drug users reflect specific individual and community needs, there is no universal definition of or formula for implementing harm reduction.” – Principles of Harm Reduction, Harm Reduction Coalition.
Portugal decriminalized all personal drug use with a cohesive national plan, turning instead to a public health approach centered around harm reduction principles. This evolved from an opioid crisis that culminated in the late 1990s. Portugal had the highest rate of overdose deaths in Europe, with an average of 360 overdoses per year across a population of 10 million people (Bramham, 2018). Individual arrests for drug possession began to increase from 4,667 people in 1991, to 6,380 in 1995, then up to 11, 395 by 1998. 61 percent of 1998 arrests were for possession or use, while 45 percent were for heroin (Van Het Loo, 2002, p. 52). The Portuguese government began to create a national drug policy called the National Plan for the Reduction of Addictive Behaviours and Dependencies around thirteen principles:
1. to reinforce international cooperation and to promote active participation of Portugal in the definition and evaluation of the strategies and policies of the international community and the EU;
2. to decriminalize the use of drugs, prohibiting them as a breach of administrative regulations;
3. to redirect the focus to primary prevention;
4. to extend and improve the quality and response capacity of the health care network for drug addicts, so as to ensure access to treatment for all drug addicts who seek treatment;
5. to extend harm reduction policies, namely, through syringe and needle exchange programs and the low-threshold administration of substitution drugs as well as the establishment of special information and motivation centers;
6. to promote and encourage the implementation of initiatives to support social and professional reintegration of drug addicts;
7. to guarantee conditions for access to treatment for imprisoned drug addicts and to extend harm reduction policies to prison establishments;
8. to guarantee the necessary mechanisms to allow the enforcement by competent bodies of measures such as voluntary treatment of drug addicts as an alternative to prison sentences;
9. to increase scientific research and the training of human resources in the field of drugs and drug addiction;
10. to establish methodologies and procedures for evaluation of public and private initiatives in the field of drugs and drug addiction;
11. to adopt a simplified model of interdepartmental political coordination for the development of the national drug strategy (IPDT replaces project Vida);
12. to reinforce the combat against drug trafficking and money laundering to improve the articulation between different national and international authorities; and
13. to double public investment to 160 million euros (at the rhythm of 10 percent a year) during the next five years, so as to finance the implementation of the national drug strategy. (Van Het Loo, 2002, p.56)
An interdisciplinary committee headed by João Goulão, the Portuguese General Director for Intervention on Addictive Behaviours and Dependencies, was formed (Drug Policy Alliance 2). By July 2001, all drugs for individual use were decriminalized (individual use is a ten-day supply or less) under Law no. 30/2000. Anyone caught using or in possession of narcotics was sent before a dissuasion commission through the Portuguese Department of Health, which operates independently from the criminal justice system (Drug Policy Alliance 4). The commission is comprised of three professional fields— legal, health, and social services sectors. Individuals attend a Commission for the Dissuasion of Drug Use (CDT) and are assessed for substance use disorder. Those who are determined to have problems with SU are offered a referral for treatment in one form or another. This can be voluntarily declined or accepted, but never mandated by the commission. The commission has the authority to implement various sanctions if the individual is unwilling to seek some type of addictions programing. (Drug Policy Alliance 4). They are as follows:
All drug-related treatment in Portugal is governed by a comprehensive framework called the National Plan for the Reduction of Addictive Behaviours and Dependencies. This national plan is subject to policy cycles, which are assessed and amended as needed as part of a flexible working model. The plan is subject to the overview of the Technical Commission Subcommittee on Monitoring and Evaluation (chaired by the National Drug Coordinator)(Santos, 2012, 20). Portugal’s National Plan regulates all treatment delivery forms, providing healthcare to substance affected individuals through the Referral Network for Addictive Behaviours and Dependencies. Service delivery falls to each regional health district through three avenues: i) publicly available specialized services, ii) non-governmental organizations, and iii) privatized treatment services (Portugal Drug Report, 2018, 17). The Ministry of Health, the Health General Directorate (DGS), and the General-Directorate for Intervention on Addictive and Dependencies (SICAD) oversee the standards for professional training and ensure that all levels of care are aggregated into an overarching framework for public policy surrounding addictions. These bodies define what is considered evidenced-based treatment and ensure that the quality of care is delivered uniformly across all institutions (Portugal Drug Report, 2018, 20). “Psychoactive drugs, addictive behaviors and drug dependencies are covered in the academic training of medical doctors, psychologists, nurses and psychosocial workers. SICAD also provides training in the domain of addictive behaviors and dependencies.” (Portugal Drug Report 2018, 20) Addiction is understood as a medical issue in which people need access to supportive services.
Portugal provides people suffering from addiction with inpatient treatment options. Therapeutic communities (TCs) in Portugal are defined as, “… specialised units that provide care to drug users who require prolonged hospitalization and psychotherapeutic and socio-therapeutic support with the purpose to promote their rehabilitation and treatment.” (Santos et. al., 2012, 144). TCs are in public and private sectors, but all are subject to government overview and inspection in regards to quality of care and service delivery. An individual’s financial situation does not preclude a person from obtaining privatized service in TCs, as “… some or all of their places can be occupied by patients coming from the public network of outpatient treatment services managed by IDT… IDT, I.P. pays or supports a number of beds. Of these 68 TC’s, 3 are public, with a total of 55 beds…The other 65 TC’s are private, with a total of 2,112 beds.” (Santos et. al., 2012, 143-144). Residential treatment facilities have 3 to 12-month residential programs; length of stay is determined specifically by the needs of the client. Those that have high rates of concurrent and comorbid disorders have the option of up to three years of care. (Portugal Drug Report 2018, 17). Each care-plan is based upon individual assessments and diagnosis of biopsychosocial needs. By 2012, outpatient treatment encompassed 72 different professional teams around the country, able to facilitate access to the three avenues of care listed above (Portugal Drug Report 2018, 17). 27,834 clients received either inpatient or outpatient treatment services in Portugal in 2016. Of that number, 3,294 were processed into inpatient treatment centers, and three of five people were first-time recipients of such services (Portugal Drug Report 2018, 18). Overdose deaths have decreased by over 80%; new HIV/AIDS diagnoses of people who inject drugs fell from 52% to 6% (Drug Policy Alliance, 6).
| 2011 | Average waiting time at National level (in days) | Responsible waiting time (in days) |
|---|---|---|
| Methadone Program | |
|
| Detoxification Unit | |
|
| Public Therapeutic Community | |
|
(Santos et. al, 2012, 69)
Outpatient services are widely available across Portugal, including various forms of opioid agonist treatment (OAT), along with harm reduction supplies. Harm reduction supplies reduce blood borne, and other communicable, diseases (Hepatitis C, Hepatitis B, Tuberculosis and HIV/ AIDS). Mobile methadone vans visit five locations per day throughout Portugal (Clay, 2018). These vans distribute OAT (methadone, buprenorphine and buprenorphine/ naloxone combination) through NGOs and non-profit organizations. Mobile units also allow for the distribution of harm reduction supplies, such as clean needles, safe smoking supplies, and condoms. Education about how to reduce the harms associated with using is also a critical aspect of prevention i.e. use drugs before alcohol (Clay, 2018). Accessibility is a key factor. Mobile units make it easy for those on OAT to access it throughout their work days. These vans also offer testing for infectious disease.
In 2000, people who used drugs accounted for 52 percent of new HIV/AIDS diagnoses (1,430 out of 2,758 cases). In 2015, it decreased to a low of 6 percent (77 out of 1,228). Since 2001, HIV-related deaths among people who use drugs have consistently fallen. Overdose deaths decreased by over 80 percent after decriminalization. In 1999, 369 drug overdose deaths were recorded in Portugal (36.2 per million); by 2015 that number had fallen to 54 (5.2 per million) (Drug Policy Alliance 6).
Abstinence is not a requirement under the harm reduction model, so clients are met where they are at, but there is special emphasis on relationship building and the reduction of stigma. Outreach teams walk the streets, distribute clean supplies, provide information, and are generally the first line of contact for a person seeking treatment.
Reintegration teams run by the IDT ensure people can access the transitional support that is needed after involvement with a therapeutic community. Reintegration teams collaborate with both staff and patients around diagnoses, education, employment, and patient goals when transitioning back into the community (Domoslawski, 2011, p.35). Stigma and homelessness are common issues that people with addictions face; social relationships with family members and friends can often be tenuous, unhealthy, or non-existent, making the recovering individual very vulnerable. The Portuguese government understands the critical need for transitional housing and employment programs as a final link in the effective treatment of addiction. Being released from treatment, and/or another institution, to the streets creates high-risk conditions for relapse. Transitional housing can range from 6 to 12 months after treatment. “In 2009, 29 apartments were operational serving 227 users.” (Santos et. al., 2010, 99).
The SICAD cooperates with companies that sponsor nine-month internships, so people can gain employment experience and transition to further employment and obtain their own housing (Domosławski, 2011, p. 35). “Obtaining and keeping an employment is a crucial step in the reintegration process…. it is also important for the self- esteem, social skills, knowledge and life experience which contribute to the self-stability, as an active and useful member of society.” (Santos et. al., 2010, 101). The Institute for Labor and Professional Training (IEFP, I.P.) and the Life- Employment Program – Programa Vida Emprego (PVE) provide avenues for sustainable employment (Santos et. al., 2010, 100). PVE specifically provides employment opportunities for those individuals who are particularly vulnerable to debilitating mental health issues (schizophrenia, schizoaffective disorder, bipolar disorder etc.) and other comorbid factors. Such individuals would otherwise have severely reduced opportunities for employment. The IEFP and I.P. employment exchange programs partner (and sponsor) with community enterprises to create sustainable integration into the community. In 2009, private companies comprised 40 % of the entities participating; local administration entities comprised 25%; and private institutions of social solidarity (IPSS) comprised another 25%; 7% were from associations; 3% participation were cooperatives and 2% were from public entities (Santos et. al., 2010, p.102). In other words, micro-companies with fewer than 10 employees employed 40% of people participating in the program. Small companies with 10 to 50 employees employed addicts 37% of the time. Medium sized companies with 50 to 250 employees participated in 10% of cases. Large companies with over 250 employees were only 5% of employers in work reintegration programs (Santos et. al., 2010, p. 103).
(Browne 2016) VICE News.
Harm reduction is fundamentally about human rights. The Portuguese model reminds Canada of three important points: 1) that people with substance use disorder have an inherent human value that deserves respect and no one person is more deserving health care than another; 2) Decriminalization of all drugs for individual use is an important element of recognizing addiction as a health issue; 3) Treatment requires multi-faceted care, such as detoxification facilities, therapeutic communities, transitional housing and employment programs. The Substance Use and Addictions Program (SUAP) delivered by Health Canada only provides $28.3 millions dollars a year to the provinces, territories, NGOs, and other stakeholders (Government of Canada, 2018). Canada has implemented some harm reduction measures, which vary by individual province, but they still fall short of the needed intervention strategies. Opening safe injection sites, providing naloxone kits, handing out harm reduction paraphernalia (i.e. clean needles and biohazard containers) and enacting good samaritan laws are only part of a rehabilitative framework. Naloxone may keep people alive after overdosing but for others, the wait time to access detox or for a bed in a TC after detoxification facility still results in death.
Many people develop an opioid addiction through legally prescribed medication for pain management from board certified physicians, often related to mismanaged prescribing, dispensing, and titration. “…Opioid dispensing levels are strongly correlated with increased mortality, morbidity and treatment admissions for substance use. Many patients were prescribed these medications and developed dependence.” (Canadian Medical Association, 2015, 1). The Canadian Government is accountable for providing adequate treatment to people for what is so freely prescribed in a legalized setting. An article entitled “Harm Reduction in Hospitals” notes that “Drug use is among the most stigmatized conditions in health care.”(Sharma et. al., 2017, p.1). Ironically, that means that the same medical system that often assists in initial opioid use disorder stigmatizes these individuals once the addiction process is triggered. Many people with substance use disorder are reluctant to seek out potentially life-saving medical care due to hospital policies, which afterwards force abstinence and continue to mismanage acute withdrawal symptoms. Forced detox can dramatically increase the potential for overdose, so hospital policies are actually putting people’s lives at risk (Rachlis et. al., 2009, p. 2). People are leaving medical facilities despite recommendation, because they feel stigmatized. If stigma exists among educated medical professionals, then it can certainly live among Canadian households and in governments. What then happens to people suffering with a treatable disorder when medical facilities become unsafe places for assistance and recovery?
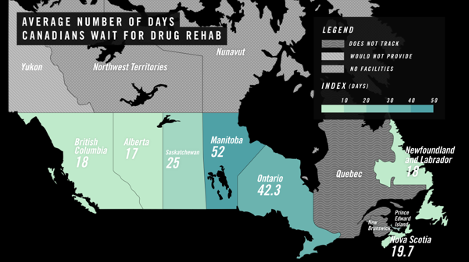
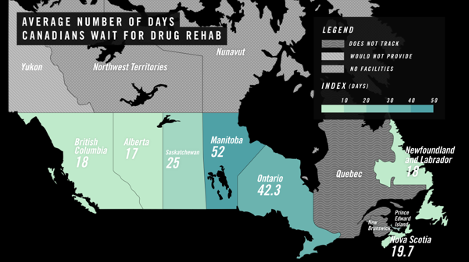
The depiction above titled, “Average Number of Days Canadians Wait for Drug Rehab” was compiled by VICE News in the absence of national tracking and statistics. However, the numbers do not always correspond to an accurate depiction of wait times for TCs, which are sometimes up to 10 months in duration (Browne, 2016). The only federally funded avenues for treatment centers are for Indigenous Peoples, through the First Nations Health Authority (they do not track wait times). The Northwest Territories does not have inpatient facilities, so people must be sent to different provinces for rehabilitation (Browne, 2016). And in places like British Columbia, accessing a provincially funded bed at a privatized treatment center requires an individual to exhaust all other options first. The reality is that that individual may die before being able to access that placement. This is a national failure of care. Wrap-around rehabilitative treatment is primarily left to the privatized sector for individuals with recovery supports based in financial privilege.
Canadian legislation must adopt the Portuguese model of public health and harm reduction to address the opioid crisis in Canada. Simply put, it is about society helping people to help themselves. This help needs to include the decriminalization of all drugs. Too often in Canada, getting out of active addiction is not a matter individual desire or willingness to do the work involved in recovery. People need increased access to beds in medical detoxification facilities, as trying to detox without medical oversight is often dangerous. People who are trying to change their lives are being released from medical and social detox facilities to homeless shelters, the streets, or other unsafe environments. They are unable to access beds at treatment centers for months at a time. Treatment centers provide people with opportunities to access vital mental health supports, learn to process emotions, begin building self-esteem, address trauma, and learn about healthy relationships to self and others. Yet many more people who have completed treatment are unable to access transitional housing in a safe, stable environment from which to build new lives. After treatment people need hope, and they need help to build a life for themselves they are afraid to loose. Integrative work programs in the formal economy help people find meaning and purpose in their lives. We have the knowledge of how to better help people afflicted by addiction, so why is Canada not implementing a wrap-around model of care similar to Portugal’s?
An opioid crisis hit Canada in the 1990s and calls to decriminalize drugs have been suggested for roughly 20 years. In the 1990s, British Columbia’s chief coroner, Vince Cain, called for the decriminalization of all drugs, identifying it as a public health issue in a 1994 report titled “Report of the Task Force into Illicit Narcotic Overdose Deaths in British Columbia” (Ferreras, 2017). “Fatal overdoses in B.C. had climbed from 39 in 1988 to 331 in 1993….Drug use became the most common cause of death for B.C. men and women aged 30 to 34. Heroin was identified in 90 per cent of cases…” (Ferreras, 2017). Fentanyl hadn’t yet hit Canadian streets. There is growing support for all drugs to be decriminalized across Canada i.e. Patricia Daly, Chief Medical Health Officer at Vancouver Coastal Health, as well as the cities of Vancouver and Toronto (Ferreras, 2017). The reality is that a Canadian citizen arrested for a small amount of an illicit substance potentially faces a criminal record, significant jail time, and loss of employment and housing. This only entrenches social barriers, making it more difficult for an individual to recover from the effects of a punitive approach to an illness. The “war on drugs” is ultimately a war on people. Decriminalizing all drugs for personal possession and providing all substance dependent individuals with wrap-around care isn’t a get-out-of-jail-free-card. Addiction is a life-long battle and staying abstinent is the same. Wrap-around care is actually the opportunity to fight that battle with the support needed for success, and all of society would be better for it.
One of the main issues in the opioid crisis is stigma. The association between immorality and addiction traces its way back to the temperance movement of the 1800s, rooted in forms of Christianity (Levine, 1978, p.7). “The clergy, especially the educated and scholarly Puritans, did most of the warning and chastising about habitual drunkenness – what they called the "Sin of Drunkenness" and the "Vice of Drunkenness."” (Levine 1978, p. 4). But Canada has, since then, decriminalized the sale, purchase, and consumption of alcohol despite its potentially dangerous effects. Why not all drugs? Canada began its own “war on drugs” under early 20th century capitalist market controls, deep-seated racist fears of non-British immigrants, and bourgeois concepts of normative society (Gordon, 2006, p. 59-60). Canada passed its Opium Act in 1908 in response to Chinese immigration, and fears that Chinese culture would bleed into the fabric of Canadian society as a corrupting influence. This 1885 police officer testimony during a government commission is primarily concerned with racial intermingling, not dangerous physical effects (Gordon, 2006, p. 63-64). “Opium is the Chinese evil…the evil is growing with the whites…principally working men…and white women prostitutes…I have seen white women smoking in the Chinese dens myself.” (Gordon, 2006, p. 64). The Canadian government was also dependent upon exploiting immigrant labor, thus it was critical to cut off any legal alternatives to income opportunities, so making opium illegal for sale or use ensured that immigrants could not function or flourish in an alternative economy, or trespass against bourgeois ideals (Gordon, 2006, p. 65). Unfortunately, this tough-on-crime approach is still being used to uphold racial order and bourgeois values. Todd Gordon writes, “…field research with police found that they often stop individuals— disproportionately people of color— who had done nothing identifiably illegal, on the pretense that they may be carrying illicit substances.” (2006, p. 69). The Canadian federal government still refuses to consider decriminalization, choosing instead to ally with the United States and their own “war on drugs” ideology. Prime Minister Justin Trudeau made Canada a signatory to President Donald Trumps “Global Call to Action on the Worlds Drug Problem.” This has led to the speculation that it is, in part, due to Canadian negotiations with the U.S. around NAFTA (Lupick, 2018). Sadly, in the U.S. during 2017, approximately 72,000 people died from illicit drug use (Lupick 2018).